Court dismisses wrongful death lawsuit against hospital where COVID-19 patient died after being switched from ivermectin to remdesivir
By isabelle // 2024-09-26
Tweet
Share
Copy

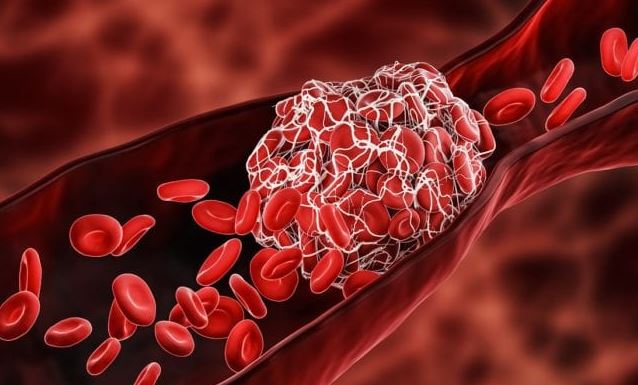
The Nevada Supreme Court has dismissed a lawsuit filed by the family of a man whose doctors switched his ivermectin treatment to remdesivir and other drugs without his permission while he was hospitalized with COVID-19.
Hal de Becker was being treated by his family doctor with ivermectin after he developed COVID-19 symptoms in spring of 2021. However, he was then admitted to the Desert Springs Hospital Medical Center out of an “abundance of caution” so he could undergo close monitoring.
The two doctors who served as his attending physicians at the hospital decided to stop giving him ivermectin and started giving him remdesivir and other drugs instead, and his condition quickly deteriorated. He died shortly after being released from the hospital.
His family says that this change was made against their wishes, which they clearly expressed to the hospital and two of the doctors treating him, and they insist the drug was switched without consulting them.
They filed a lawsuit, suing the doctors and the hospital itself for wrongful death and negligence. They maintain that the physicians and hospital were aware of the scientific evidence demonstrating the effectiveness of ivermectin against the virus but chose remdesivir instead in decisions that they believe were influenced by the media and political beliefs.
They also claim that the hospital and the doctors violated the family's right to informed consent when they failed to consult with them or his family doctor about the decisions they made about his treatment.
Hospital claims PREP Act protects them
The lawsuit was dismissed by the Nevada Supreme Court, who ruled that the Public Readiness and Emergency Preparedness (PREP) Act gives medical professionals and healthcare institutions immunity from liability for any claims of loss that are “caused by, arising out of, relating to, or resulting from the administration to or the use by an individual of a covered countermeasure.” These covered countermeasures include not only medications and vaccines but also devices and other products that have been authorized to treat patients in declared medical emergencies. According to the court, the man's family does not have grounds to sue because remdesivir is considered a covered countermeasure. However, they added that even if the PREP Act was not applicable in this case, the fact that the family did not provide some specific legal documents that were needed in an affidavit to prove professional negligence would have put the case in jeopardy either way. The family has already appealed the dismissal.PREP Act helps doctors get away with violating patients' fundamental rights
Unfortunately, the PREP Act offers broad legal protection for doctors, hospitals and pharmaceutical companies even when they are violating patients' fundamental rights. Some legal experts believe that the case should serve as an example of why legislative action is needed to prevent these acts from causing damage. Children's Health Defense General Counsel Kim Mack Rosenberg said: “The decision illuminates the way in which PREP has essentially run roughshod over other laws, including here, state informed consent law.” She added that a classification of a product shouldn’t overrule a person’s rights to make decisions about their own healthcare. “It is concerning that simply because a pharmaceutical product is defined as a ‘covered countermeasure,’ doctors can ignore, without repercussions, an obligation to obtain informed consent. The status of a product should not determine a patient’s rights to make a decision about whether or not to receive a treatment,” she said. Sources for this article include: ChildrensHealthDefense.org ChildrensHealthDefense.orgTweet
Share
Copy
Tagged Under:
freedom big government informed consent health freedom Dangerous Medicine outrage bad doctors badhealth badmedicine wrongful death dangerous doctors liberty covid-19 ivermectin remdesivir PREP Act hospital homicide Public Readiness and Emergency Preparedness Act
You Might Also Like
Coalition of gun owners for Harris-Walz has an average of only 8 members per state
By Laura Harris // Share
Unearthed clip proves once and for all that FEMA has been hopelessly castrated by the left…
By News Editors // Share
Prepper projects: Crafting your own rainwater collection system
By HRS Editors // Share
Recent News
A new front in the gun debate: Home inspections proposed in Minnesota
By willowt // Share
The Luciferian Endgame: How Satanic forces are engineering global collapse
By kevinhughes // Share
Texas AG takes action against Chinese-linked companies over national security concerns
By patricklewis // Share